Branchial Cleft Anomalies in Children: How Can Parents Detect Them Early?
Among pediatric head and neck disorders, congenital conditions dominate.
Branchial cleft anomalies account for 20–30% of congenital neck masses in children, second only to thyroglossal duct cysts. Yet, their clinical complexity and treatment challenges often surpass other conditions.
01 What Are Branchial Cleft Anomalies?
Branchial cleft anomalies arise from abnormal development of the
branchial apparatus (pharyngeal pouches, clefts, arches) during weeks 3–8 of embryogenesis. These defects lead to cysts, fistulas, sinuses, or skin tags due to incomplete closure of cervical sinuses, residual pharyngeal pouches, or ruptured branchial membranes.
02 Risks of Branchial Cleft Anomalies
Cosmetic Concerns: Visible neck masses, skin pits, or scars.
Infection: Recurrent abscesses, cellulitis, or life-threatening sepsis.
Psychological Impact: Social stigma from visible deformities or surgical scars.
Academic Disruption: Frequent infections and hospital visits may interrupt schooling.
03 Classification & Features
By Branchial Arch Origin
First Branchial Cleft Anomalies
Location: Ear region to upper neck (Pochet’s triangle).
Types:
Fistulas/sinuses: Connect to external ear canal or middle ear.
Cysts: Painless masses near the ear, prone to infection.
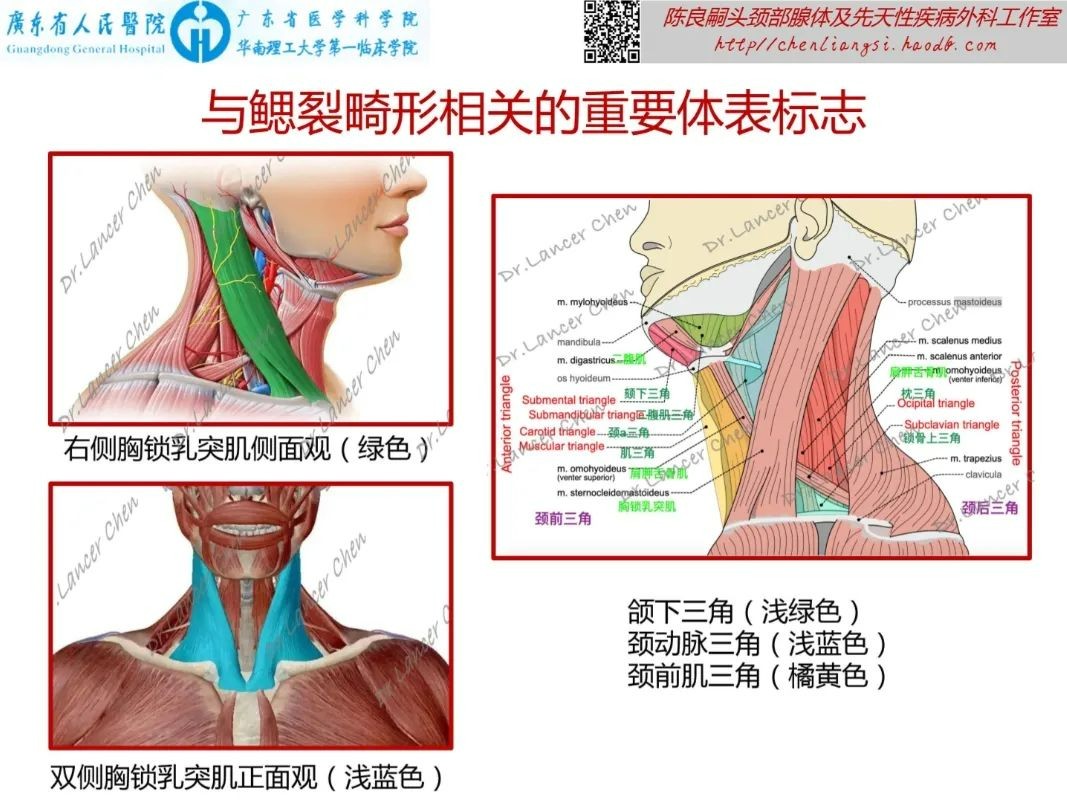
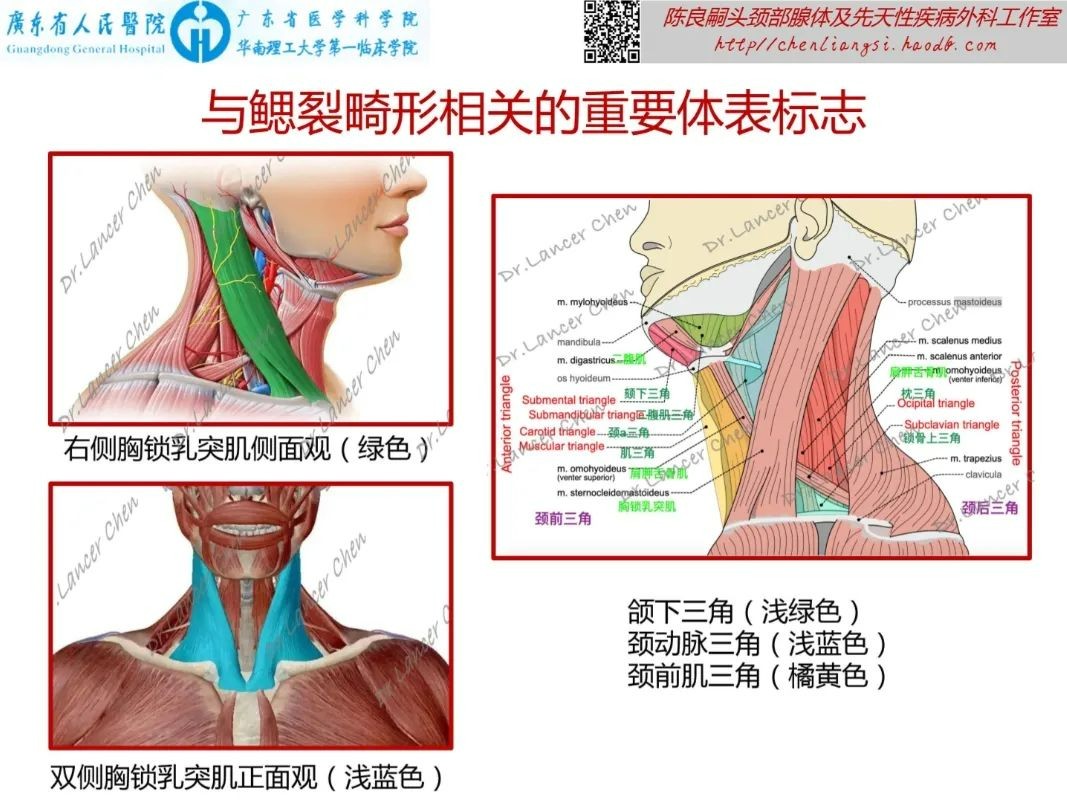
Second Branchial Cleft Anomalies
Location: Upper neck along sternocleidomastoid muscle.
Types:
Cysts (90%): Painless masses in carotid triangle.
Fistulas (10%): External opening on neck skin, discharging mucus.
Pyriform Sinus Fistula
Location: Lower neck (left-sided in 90%).
Symptoms: Deep neck abscesses, suppurative thyroiditis.
Sternoclavicular Sinus
Location: Overlying sternoclavicular joint (left-sided).
Features: Tiny skin pits with cheesy discharge.
Branchial Skin/Cartilage Remnants
Location: Side of neck or cheek (e.g., cervical accessory tragus).
Associated Syndrome: Branchio-Oto-Renal Syndrome (BORS)
Triad: Hearing loss, branchial anomalies, renal dysplasia.
88% of BORS patients have hearing impairment; 60% have branchial defects.
04 Early Detection Tips for Parents
Inspect: Check for skin pits, lumps, or asymmetry from ear to collarbone.
Palpate: Gently feel for masses; note tenderness or discharge.
Monitor: Recurrent neck abscesses or ear infections warrant specialist evaluation.
05 Navigating Medical Care
Branchial anomalies often fall into a "diagnostic gray zone" due to overlapping specialties:
Key Specialists: Otolaryngologists, pediatric surgeons, or dedicated head and neck teams.
Avoid Pitfalls: Incomplete resection (e.g., missing deep tracts) raises recurrence risk.
Renshu ENT Hospital (Guangzhou) now offers a
Branchial Anomaly Clinic led by national experts to streamline diagnosis and reduce recurrence.
Takeaway
Early detection prevents complications like sepsis or permanent scarring.
Seek
experienced multidisciplinary teams for complex cases.
Your vigilance today safeguards your child’s health tomorrow.