The clinic door gently opens again. A mother walks in holding her child’s hand, brows furrowed: "Doctor, my child always snores and breathes through their mouth while sleeping. Is it adenoid hypertrophy?"
This scene is all too familiar to ENT doctors! Seeing the child’s tired face from poor sleep, hearing the parents’ worries—Should we have surgery? What happens after surgery? Will delaying surgery harm the child?
Don’t worry. Let’s start with the
6 most frequently asked questions in the clinic. We’ll break it down to help you understand tonsil and adenoid surgery.
Q1: If my child snores and breathes through their mouth while sleeping, does it definitely mean adenoid hypertrophy?
Answer:
Not necessarily!
The cause of this "blockage" could be a single issue or multiple problems:
Nasal Obstruction: Diseases like rhinitis, sinusitis, or nasal polyps block nasal airflow, forcing mouth-breathing.
Tonsil/Adenoid Hypertrophy: Repeated inflammation causes pathological enlargement, blocking the oropharyngeal or nasopharyngeal airway.
Habitual Mouth-Breathing: Even after curing the initial disease, long-term mouth-breathing alters jaw muscles and temporomandibular joint structure, maintaining the habit.
Key point: Don’t guess! See an ENT specialist to identify the true cause.
Q2: Is surgery always necessary for adenoid hypertrophy? Can it be treated conservatively?
Answer:
Core principle:
Focus not on size but on symptoms!
If hypertrophy doesn’t affect normal development, conservative treatment (medication, physical therapy) may suffice. If it impairs development, surgery is usually recommended after evaluation, regardless of size.
Surgery indications:
Causes snoring, mouth-breathing, breath-holding, or sleep apnea affecting brain development.
Causes poor sleep (frequent waking), reducing growth hormone secretion.
Causes long-term mouth-breathing leading to dental malocclusion ("adenoid facies").
Causes speech disorders affecting language development.
Causes recurrent/persistent secretory otitis media affecting hearing.
Causes recurrent/chronic sinusitis due to blocked posterior nostrils.
In short: Symptom severity matters more than adenoid size! Follow your doctor’s advice.
Q3: Will removing tonsils/adenoids make my child get sick more easily? Weaken immunity?
Answer:
This is a major misunderstanding!
Immune markers may dip slightly short-term post-surgery, but this doesn’t cause long-term immune damage.
(Image source: Online. Removed if infringement occurs)
The pharynx has the "Waldeyer's ring" (adenoids, palatine tonsils, lingual tonsils). Removing adenoids or partial/full tonsillectomy leaves enough lymphoid tissue for immune defense. Other mucosal lymphoid tissues compensate, restoring immune function.
Stop blaming the tonsils and adenoids!
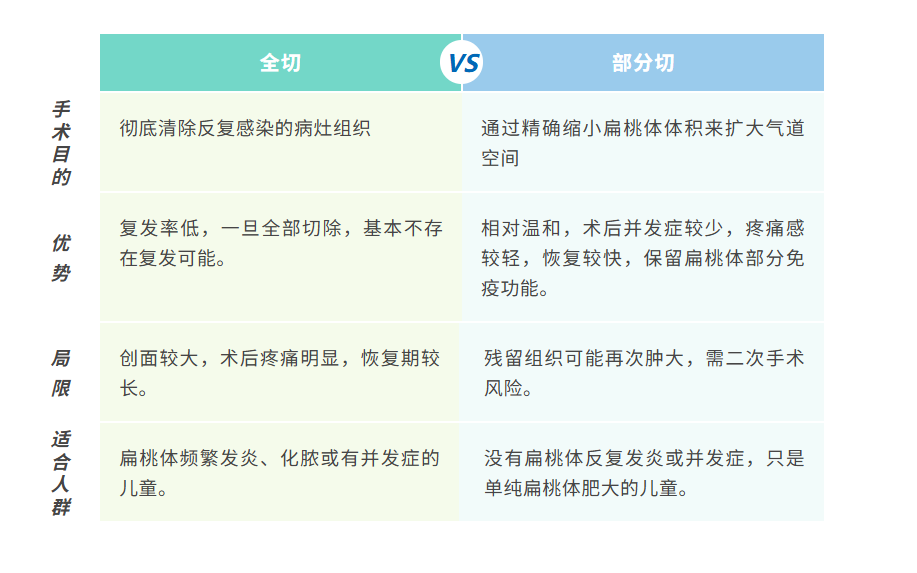
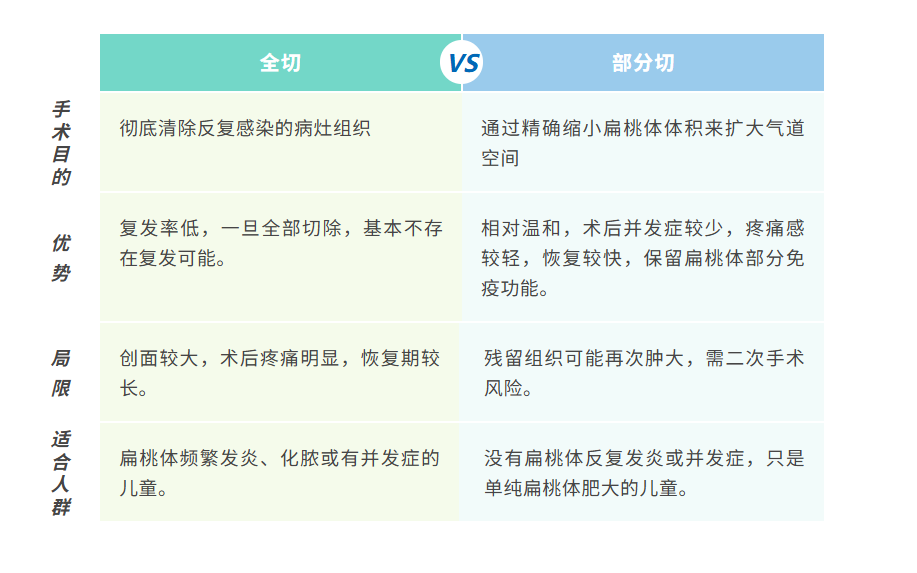
Many parents also hesitate: Full or partial tonsillectomy? Compare below:
 Every child’s healthy breath carries boundless growth potential.
Every child’s healthy breath carries boundless growth potential.
TreeENT Health understands the weight of a child’s development and every family’s hopes.
Driven by this responsibility,
the TreeENT Pediatric ENT Expert Team pursues excellence!
TreeENT Health’s pediatric ENT team gathers senior specialists from the Yangtze River Delta and Greater Bay Area. All experts have extensive clinical and surgical experience. Using advanced HD imaging and coblation technology, we ensure precision from evaluation to surgery. The team has completed
over 10,000 pediatric tonsil and adenoid surgeries.
Limited space, we stop here.
Post-op recovery? Diet? Side effects?
We’ll address post-operative concerns next week.
TreeENT Health – Dedicated to Children's Tonsil & Adenoid Health
Protecting every child’s free breath.